Casting assumptions aside
Uncovering the mysteries of seniors’ mental health care

January 4, 2017
By Karen Diaper, Communications Manager, Covenant Health
For Dr. Lori Harper and Dr. Candace Walker, every day at Villa Caritas, Alberta’s only stand-alone geriatric mental health hospital, presents opportunities to delve into each patient’s unique story and experience.
“The simplest thing can be so complicated,” explains Candace, who has been a geriatric psychiatrist with Covenant Health since the facility opened in January 2011. “We have to be creative and prioritize, and always think outside the box.”
Lori, a clinical psychologist who has worked in geriatric psychiatry for 20 years, adds, “We sometimes feel like detectives when trying to uncover what is going on with our patients.”
One of their goals is to figure out what will provide the best quality of life for a patient and their family.
Most of the patients at Villa Caritas have dementia that can range from mild to severe. There are common themes and typical elements, but every case and every family is unique.
The team starts from scratch with each patient; there are no assumptions that medical files are correct or complete.
“We have the benefit of an inpatient setting where we can observe patients day in, day out,” says Candace. “Often, the medical and the psychological go hand in hand. By doing a thorough medical review, we can ensure there isn’t anything reversible or medical contributing to their psychiatric presentation.”
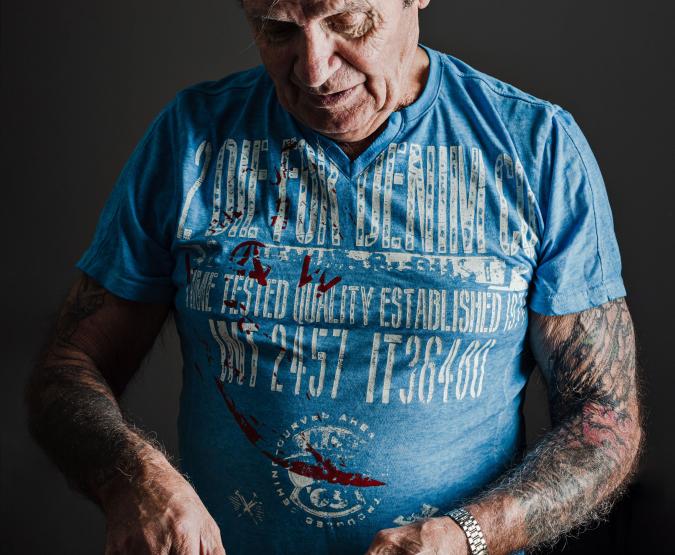
This was indeed the case for one patient, Jerry Salvino, 75. He was admitted with dementia, and prior testing showed extremely poor functioning. Jerry was transferred into Candace's care, and she spent time observing him on the unit.
“Jerry’s case was unique in many ways,” she says. “He was functioning extremely well and was helping other patients on the unit, and presenting as cognitively intact. Nothing I observed fit with prior reports and test results, so I felt it warranted a second look.”
“Jerry repeated psychological testing, and his assessment results showed average functioning on the majority of measures used,” says Lori. “We did a capacity assessment and he did well. It turned around for Jerry at that time. He felt he was on this path to independent living where alternatively he may have had his decision-making power taken away.”
Jerry, who now lives independently, speaks fondly of his two doctors.
“Jerry worked with us to find an appropriate place for him to live,” says Lori. “He was also very accepting of supports and services we were offering to him in followup.”
“It took these women to help me see the light,” Jerry says. “They treated me as equal to everyone else at Villa Caritas. In three months, they turned my life around. I call them the A-Team.”
“Some cases can change and the initial assumptions may be wrong,” notes Candace. “For example, in Jerry's case, if I'd just looked at the testing and diagnosis of the previous files, he would have had alternate decision-making put in place. What's important is the fact that the clinical picture can change and we need to be open to those possibilities.”
But in Jerry’s words, “These ladies never gave up on me. It’s an exciting time. I should have started this journey when I was 30.”