Breastfeeding
Breastmilk is the only food and drink your baby needs for the first six months of their life for healthy growth. At six months, start giving your baby solid foods. We suggest you keep breastfeeding your baby for two years or more.
Every baby is unique. It will take time and practice for you and your baby to learn to breastfeed. For most moms, it takes four to six weeks to feel confident breastfeeding.
What to expect after delivery
After your baby is born, we will help you place them against your skin for at least the first hour. Skin-to-skin care helps:
- you and your baby bond
- calm your baby
- boost your milk supply
- adjust your baby's temperature, heart rate and blood sugars
If you are unable to practice skin-to-skin care after the birth, your partner can practice skin-to-skin care with your baby.
Benefits of breastfeeding
- fewer or less severe ear infections and allergies
- lower risk of sudden infant death syndrome or illnesses involving breathing or digestion
- lower risk of having diabetes, certain childhood cancers and obesity
- natural child spacing through the lactation amenorrhea method (LAM)
- lower risk of too much bleeding after birth and of breast and ovarian cancer for the birthing parent
Breastfeeding basics
- It is your right to breastfeed anywhere, anytime.
- Feeding often and for as long as your baby wants will help you make breastmilk. The more breastmilk your baby drinks, the more milk you will make.
- Let your baby guide the number and length of feedings. Breastfeed whenever your baby shows signs of hunger. They will stop feeding when they are full.
- Offer the breast before your baby cries by watching for early signs of hunger (sucking motions, smacking lips, putting their fist or fingers in their mouth or searching with an open mouth).
- It is normal for breastfed babies to feed at least eight times in 24 hours.
- All babies grow differently. Growth spurts often happen at three weeks, six weeks, three months and six months.
- Find a breastfeeding buddy. This is someone who has had a positive breastfeeding experience and can help you. They can share breastfeeding knowledge to help you on your breastfeeding journey.
Breastfeeding in the first 24-48 hours
Don’t limit your baby’s feeding time. Watch for feeding cues, and let your baby breastfeed until they let go of the breast.
A baby should feed every two or three hours, but babies often want to feed more often, even every hour, especially on the second day. This is normal and is not a sign of low milk supply. It means your baby is getting used to their new world.
Don’t worry about your milk supply. During your pregnancy, you made plenty of colostrum (see below) for your baby to drink at this time. The frequent feedings will help you make mature milk.
Babies feed better when they can touch or feel your skin. Take your baby’s blankets and baby mittens off for feedings. Your baby’s touch will help them focus on feeding and boost your milk supply.
Colostrum
Colostrum, sometimes known as liquid gold, is a thick sticky yellow milk that you produce during pregnancy and during the first few days after birth.
Colostrum contains large amounts of living cells that protect against bacteria and viruses. It acts as a baby's first vaccine.
Even though your body makes a small amount of colostrum, it is high in nutrition and is all your baby needs in the first few days after birth.
Normal feeding
At first your baby may be sleepy. You may need to try changing their diaper or placing them skin-to-skin to help them wake up and feed.
It is normal on the second night for your baby to feed often and cry if taken off the breast. This can be stressful for new parents but is normal for newborns.
How often to breastfeed
Breastfeeding early and often will help you make enough milk for your growing baby. The more often you feed, the more milk your body will produce.
Babies feed often during the evening and sometimes through the night. This also helps to boost your milk supply.
Try to breastfeed at least eight times in 24 hours. You may feed more if your baby shows signs of hunger.
Holding your baby
Here are a few ways you may choose to hold your baby while breastfeeding.
Cradle hold
Comfortable once baby latches on
Laid-back nursing position
Used from first breastfeeding and great for everyone
Cross-cradle hold
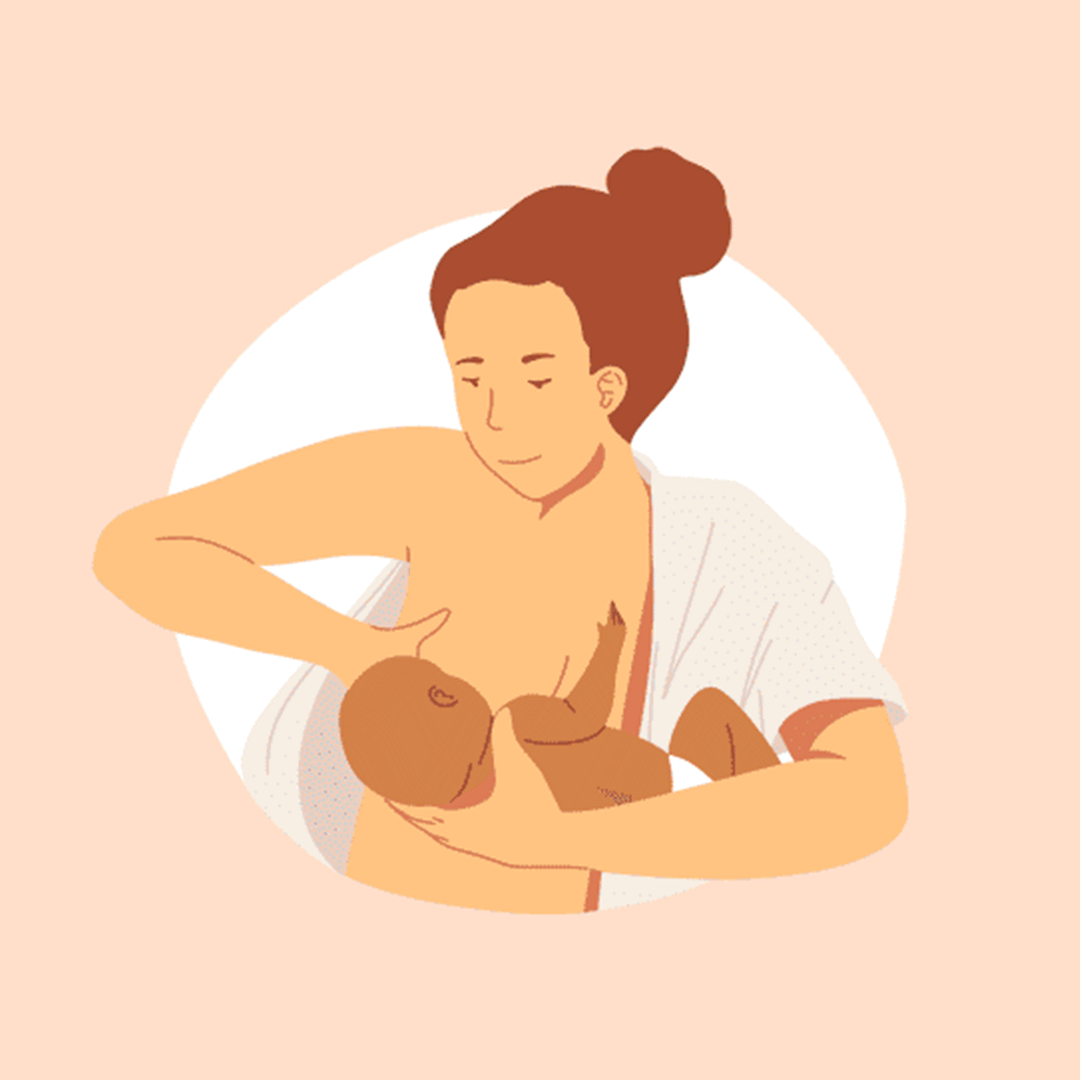
Helpful for preemies, newborns or babies who have trouble latching on
Side-lying position

Great for night-time feedings and C-section recovery
Football hold
Good for nursing twins, C-section recovery, large breasts and flat or inverted nipples
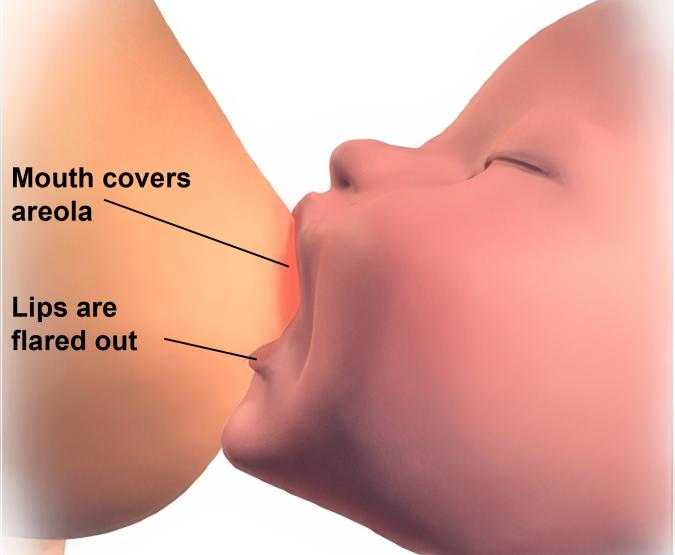
Helping your baby latch
Breastfeeding is more comfortable when your baby has a good latch to your breast. Try these tips to help your baby latch well.
- Make sure your baby is facing you, tummy to tummy and face to breast.
- Support your baby behind their neck and shoulders. Do not push on the baby’s head.
- Wait for your baby to open their mouth wide like a yawn, with their tongue down.
- Bring your baby to your breast chin first, with their head slightly tipped back. The baby’s nose will be close to your breast but will still have room to breathe.
- Your baby will have a large portion of areola (the area around your nipple) in their mouth when they have a good latch. The baby’s cheeks will look full and rounded.
Signs that your baby drinks enough
- You can hear or see your baby swallowing and can see jaw movements.
- You may hear your baby make a “ca” sound.
- Your baby seems content and satisfied after feeding.
- Your baby pees and poops the right amounts based on their age.
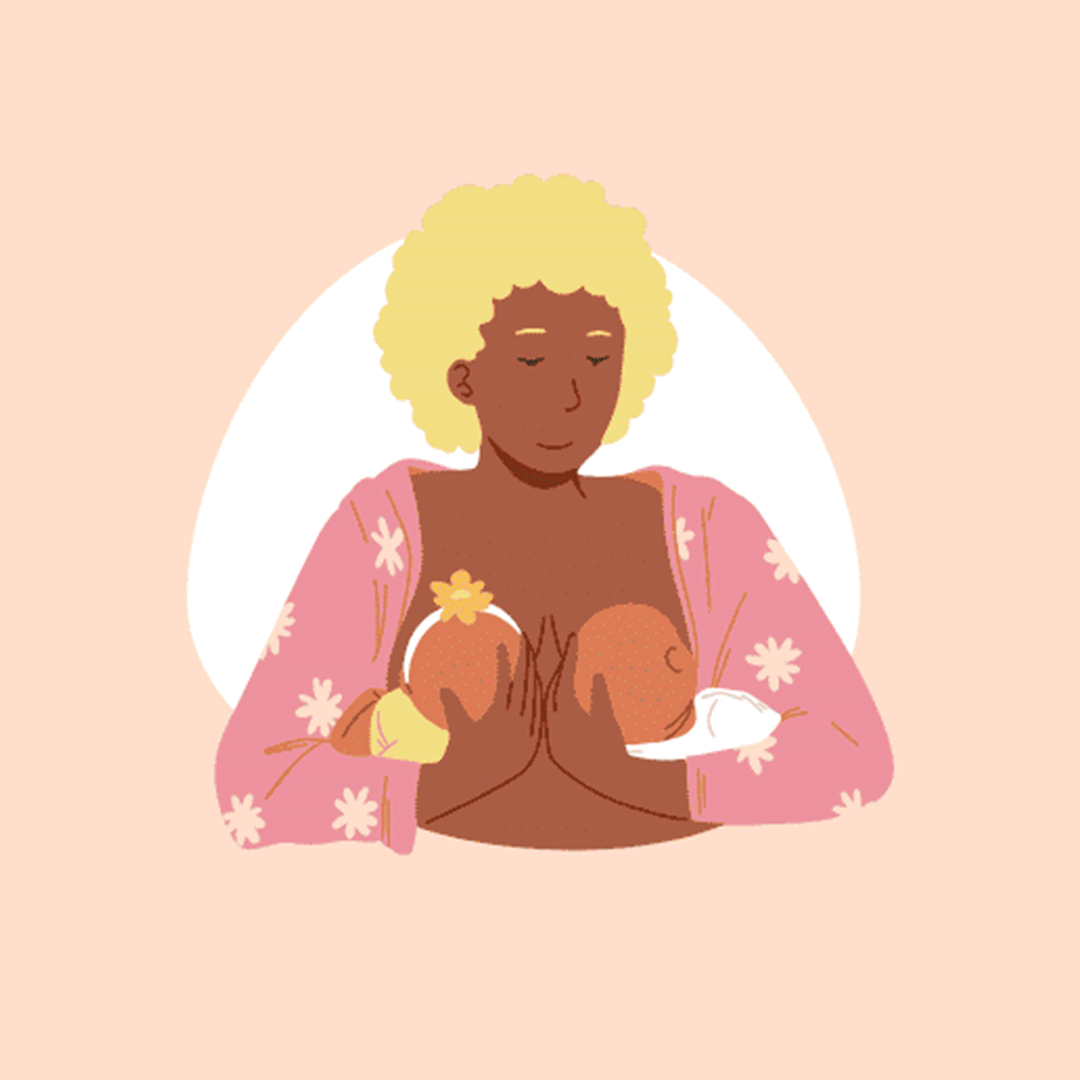
Expressing and storing breastmilk
You can express breastmilk by hand or with a breast pump. Releasing milk from your breasts will help your milk supply.
You may need to express your breastmilk to:
- feed your baby if they aren’t able to latch
- feed your baby if they are sick or preterm
- make sure your baby has breastmilk while you are away from them
- soften your breasts if they are full or engorged
- keep your milk supply if you cannot breastfeed
How to express your breastmilk by hand
- Start by washing your hands well.
- Before you begin, try placing a warm cloth or pad on your breast and gently massaging it in circular motions — about as light as petting a cat. This can help your milk start to flow.
- Take a few deep breaths and try to relax. This helps your body release oxytocin, the “love, labor and lactation” hormone that helps milk flow.
- If possible, hold your baby skin-to-skin. This also helps your body release oxytocin. If you're separated from your baby, try looking at a photo, FaceTiming, smelling their clothing or listening to their sounds.
- You can also gently stroke and massage your breasts to help the milk flow.
- Put your thumb and index finger one to one and a half inches outside your areola. Press your thumb and index finger back toward your chest.
- Roll your thumb and index finger toward your nipple. Avoid pulling on your nipple.
- Relax your fingers on your breast.
- Repeat these steps, moving your fingers around your entire breast. Keep doing this until the milk stops flowing. Switch hands if you need to and move from one breast to the other.
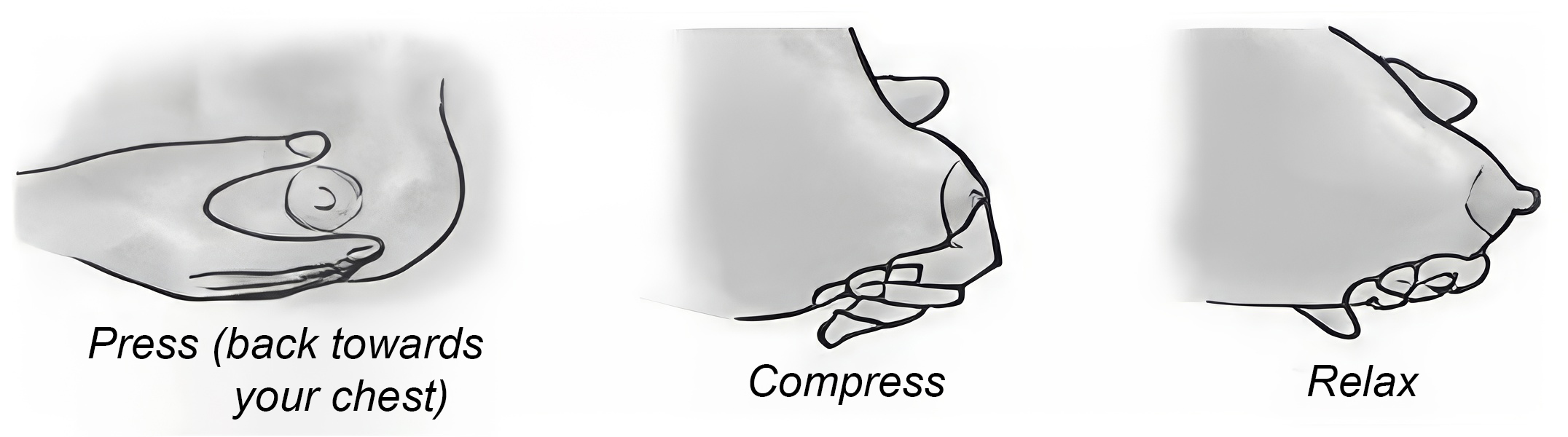
If your baby is not latching or is sleepy at the breast, or if you are separated, try expressing your milk every two to three hours to help keep your supply going.
Using a breast pump
Sometimes you may need to use a breast pump to give your baby milk, just like you would with hand expression. You can use a manual pump (that you squeeze by hand) or an electric pump (that uses power to help express milk).
There are many types of pumps. If you are not sure which one is right for you, talk to your healthcare provider or a lactation consultant. They can help you choose a pump that fits your needs.
When picking a pump, try to find one that:
- is easy to clean
- is simple to use
- has spare or replaceable parts
- suctions your milk on and off in cycles, with rests in between
- is comfortable to use (it does not pinch or hurt your breasts)
- is portable if you need to pump on the go
Hand pumps
Hand pumps (also called manual pumps) do not need electricity. They can be helpful if you only need to pump once in a while or when you're away from home.
Most breast pumps come with a flange size of 21 millimetres, 24 millimetres or 27 millimetres. These sizes might not fit you properly. A poor fit can make pumping uncomfortable or not work well. If you're not sure which size is right for you, ask your healthcare provider or lactation consultant.
Electric pumps
Electric pumps come in many styles. Some are small and you can carry them with you. Others are larger and stronger. They usually come with a 21-millimetre, 24-millimetre or 27-millimetre flange, which may not be the best fit for you. Getting the right size can make pumping more comfortable and help you get more milk.
Storing breastmilk
It is important to know how to store your breastmilk safely.
| How milk is stored | How long it can be stored |
|---|---|
| Room temperature | Four hours |
| Insulated bag with frozen gel pack | 24 hours |
| Fridge | 48 hours |
| Freezer compartment of a one-door fridge | Two weeks |
| Separate freezer compartment in fridge | Three to four months |
| Deep freezer (-18° C) | 12 months |
Thawing frozen breastmilk
Always use the breastmilk that has been frozen longest first. To thaw breastmilk, put it under warm running water or in the refrigerator.
Thawed breastmilk must be used within 24 hours. After 24 hours, it is not safe for your baby and you must throw it out. Never refreeze breastmilk.
Do not thaw or warm breastmilk in a microwave. Microwaves heat unevenly, forming hot spots that can burn your baby. The microwave can also destroy parts of the breastmilk that your baby needs.
Ways to feed your baby breastmilk
Learning to breastfeed takes time for both you and your baby. In the early days, your baby may have trouble latching or staying awake at the breast. This is normal.
If your baby is not able to breastfeed yet, you can still give them your breastmilk in other ways. This helps keep your milk supply going while your baby learns to feed at the breast.
Here are some options
- Spoon feeding: Your baby is held upright and can lap or sip the milk slowly from a spoon.
- Cup feeding: Your baby sips the milk at their own pace.
- Using a syringe or dropper: Your baby drinks small amounts of milk at their own pace.
- Bottle feeding: Your baby gets breastmilk through a bottle.
Cup feeding
You can use a cup to feed your baby when you are not able to breastfeed. You might choose to cup feed to:
- give your baby extra supplements along with breastfeeding
- avoid nipple confusion
You can always ask your nurse for help.
Equipment
To cup feed, you will need:
- a small clean cup
- a clean cloth
How to cup feed
To feed your baby using a cup:
- Pour 5-10 millilitres of breastmilk into a medicine cup.
- Wrap your baby loosely so that their hands cannot swipe the cup. Your baby should be calm and alert and giving cues that they are ready to feed.
- Hold your baby close to your body in an upright position. Use your arm or hand to support their head, neck and body.
- Gently tap your baby's lower lip with the cup. This will tell them that it is time to eat.
- Hold the cup so the rim touches the corners of the baby’s upper lip and gums. Let the rim rest lightly on the baby’s lower lip without pressing down. Make sure the baby’s tongue can move freely under the edge of the cup.
- Tip the cup so that milk touches the baby’s lips. Your baby should begin to lap the milk from the cup. Do not pour milk into your baby’s mouth.
- Keep the cup in the same tipped position. Do not move it away when the baby pauses. Only pull it back if the baby moves away. Let your baby start drinking again when they are ready and follow their pace.
- Watch your baby and follow their cues.
- Burp your baby as you would in any other feeding.
- When your baby has had enough, they will stop taking more.
You will know your baby is full if they:
- close their mouth
- turn their head away from the cup
- relax their hands
- use hand motions or make sounds
Tips
- Offer your baby your breast first, then give them extra milk if needed.
- Pump right after breastfeeding (10-15 minutes per breast).
- Try to finish each feeding and pumping in about an hour or less so everyone can rest.
- Watch your baby’s behaviour. The number of wet and dirty diapers and your baby’s weight gain will show you if your baby is getting enough food.
Spoon feeding
Spoon feeding is a good way to give your baby small amounts of breastmilk, especially in the early days.
To feed your baby with a spoon
- Express a few drops of colostrum or breastmilk into a clean spoon. You can also pour a small amount into the spoon.
- Hold your baby upright. Do not feed them while they are lying flat.
- Gently bring the spoon to your baby’s lips. Let them lap or sip the milk at their own pace.
- Give your baby time to swallow before offering more.
Bottle feeding breastmilk
You may use bottle feeding to help your baby get breastmilk. Sucking from a bottle is different from breastfeeding. Bottle nipples release milk right away and are easier for babies to suck. This can change how your baby breastfeeds. Some babies may bite or push the breast out if they get used to fast bottle flow.
If you use a bottle, talk to your healthcare provider or lactation consultant about paced bottle feeding. This method helps your baby feed more like they would at the breast.
When breastfeeding isn’t an option
You may not be able or you may choose not to breastfeed. Whatever your situation, we’re here to support you.
If you decide to feed your baby with formula, it’s important to have the information you need to make the choice that feels right for you and your baby.
If you use a bottle, consider trying paced bottle feeding. This method lets your baby take breaks and feed more slowly, much like how they would at the breast. It can help prevent overfeeding, which is common with bottle feeding.
You can learn more about formula feeding from MyHealth.Alberta.ca Network.
Breast health concerns
Breast engorgement
Breast engorgement means your breasts are too full. It happens when milk is not taken out of the breasts often enough or in large enough amounts. Engorgement usually happens between two and five days after birth.
One or more of your breasts may be engorged if:
- it is very full, heavy, hot, red, painful or tender
- it feels lumpy, including the breast tissue under your arm
- the nipple is flatter than usual
Engorgement can happen if:
- your baby is not latching or feeding well
- your baby goes longer than usual between feeds (for example, sleeps through a feed)
- you are pumping or hand expressing after feeds when it’s not needed
- your breast pump doesn’t fit well and isn’t removing milk properly
Protect your breasts
You can keep your breasts from becoming engorged by:
- latching your baby correctly to the breast
- feeding your baby at least eight to 12 times in 24 hours, or more if they demand it
- feeding your baby when they show early feeding cues
- not using soothers or bottles
- expressing or pumping your milk if your baby is having trouble latching, you are away from your baby or your breasts feel too full for your baby to latch comfortably
Caring for engorgement
Before feeding
If your milk is dripping or you can express it, apply warm, moist heat with a cloth or pad to your breasts for two to five minutes. Massage your breasts gently in a circular motion (start under your arm and move toward the nipples). Then try to hand express or pump your milk.
Between feedings
- apply a cold cloth or pad to your breasts
- wear a bra that gives your breasts good support
- take pain medicine every 20 minutes before feeding
When you need help
Call the Healthy Beginnings Hotline at 780.413.7990 or your lactation consultant if you need help with breastfeeding or breast engorgement.
Thrush
Thrush (candidiasis) is an infection caused by a fungus or yeast called Candida albicans.
Candida thrives in warm, wet places. Mothers and babies who have had antibiotics in labour, or while breastfeeding, are at higher risk for thrush.
Signs of thrush in mothers
- red, sore, cracked, itchy, burning or painful nipples that may have white patches
- red, swollen, flaky/scaly or shiny-looking areolae (the area around your nipples)
- nipples that do not heal, even though your baby is not having problems with positioning, latching, sucking or swallowing
- sudden pain in your nipples that may feel like a paper cut
- severe nipple pain during and after breastfeeding
- sharp, shooting or burning pain in your breast during or after feeds
Signs of thrush in babies
- white patches on the tongue, gums, inner cheeks or soft palate that cannot be wiped off
- changes in breastfeeding behaviour, such as not wanting the breast or uneven sucking
- change in temperament (the baby may become gassy or cranky)
- slow weight gain
- diaper rash with raised, red, sore-looking pustules (bumps) or red, scalded-looking buttocks
Adapted from Alberta Health Services STORC: Managing Breastfeeding Challenges and Supplementation Module (2017, June, rev. 2018, April).
Duct narrowing (blocked ducts)
You may have a blocked duct if you notice:
- a red or sore spot on one or both of your breasts
- tenderness or pain in one area of your breast
- a feeling of pressure or discomfort in your breast between feedings, like something is stuck
Blocked ducts can happen when:
- your baby is not latching or feeding well
- your baby goes longer than usual between feeds
- you are pumping or hand expressing after feeds when it’s not needed
- your breast pump doesn’t fit properly and isn’t removing milk well
How to care for a blocked duct: The B.A.I.L. method
If you have a blocked duct, try the following:
- Breast rest: Feed or pump as you normally would. Do not add extra pumping or feeding sessions to try to “clear” the duct. This can make things worse.
- Analgesic and anti-inflammatory: On your doctor’s advice, use pain medicine like acetaminophen and an anti-inflammatory like ibuprofen to reduce swelling and discomfort.
- Ice (cold compress): Apply a cold cloth or ice pack after feeding or pumping to help reduce swelling.
- Lymphatic drainage: Gently stroke your breast (as lightly as petting a cat) away from your nipple toward your collarbone or armpit. This helps move fluid out of the area. Avoid stroking hard or deeply, using heat or suctioning with pumps or other devices.
Seek help: Always contact your healthcare provider if you think you have a blocked duct. The B.A.I.L. method is helpful, but it should not replace medical advice.
Mastitis
Mastitis is inflammation (swelling, redness and soreness) or infection in one or both breasts. It can happen when a blocked duct is not treated or if bacteria gets into the breast.
There are two types:
- inflammatory mastitis — swelling and pain without signs of infection
- bacterial mastitis — swelling and pain with signs of infection
You can still breastfeed if you have mastitis. The infection cannot be passed to your baby, but your milk flow may slow down, and your baby may be fussier at the breast. This usually improves as you start to feel better.
Signs of mastitis
- redness in one area of the breast
- swelling and tenderness
- fever
- chills
- fast heartbeat
If you have these symptoms, contact your doctor right away or go to the emergency room. Mastitis needs medical treatment.
The B.A.I.L. method can help relieve symptoms of mastitis, but it should be used along with medical care.